Endometriosis is the name given to the condition where cells, similar to the ones in the lining of the womb, are found elsewhere in the body. Each month these cells react in the same way to those in the womb, building up and then breaking down and bleeding. But unlike the cells in the womb that leave the body as a period, this blood has no way to escape causing chronic pain.
Endometriosis affects approximately 176 million women, Endometriosis can affect anyone assigned female at birth, including women, trans men, non-binary and intersex individuals, of reproductive age worldwide.
What is Endometriosis?
During the menstrual cycle, the body goes through hormonal changes each month. Hormones are naturally released which cause the lining of the womb to increase in preparation for a fertilised egg. If pregnancy does not occur, this lining will break down and bleed – this is then released from the body as a period.
In endometriosis, cells similar to the ones in the lining of the womb grow elsewhere in the body, often on other organs such as the bowel, bladder or ovaries. These cells react to the menstrual cycle each month and also bleed. However, there is no way for this blood to leave the body. This can cause inflammation, pain and the formation of scar tissue.
In the UK, 1.5 million women suffer from this condition. Endometriosis can have a significant impact on a person’s life causing chronic pain, fatigue, depression, isolation, affecting sexual intercourse and making it difficult to conceive. The condition also restricts the amount and kind of work you are able to do.
It's a very difficult condition to manage as there is no cure. So, treatment comes in the form of pain management, various injections including menopause inducing hormones, and laproscopic procedures where a consultant operates to remove the endometrial cells. For some women, a hysterectomy may be the answer to eradicating endometriosis. This works for some women. It doesn't work for others. Everybody's body will have a different reaction to the condition.
The fight for diagnosis & treatment
When researching this article we were told by many women with endometriosis that they struggled to be heard by many clinicians, friends and even family members. That they were dismissed, not believed and passed from one inappropriate appointment with the wrong specialist, to the next. Is this down to misconception, a lack of understanding, an unwillingness to listen? Putting the reason why aside for the moment, being passed from pillar to post often means that women are waiting for an average of eight years for a diagnosis.
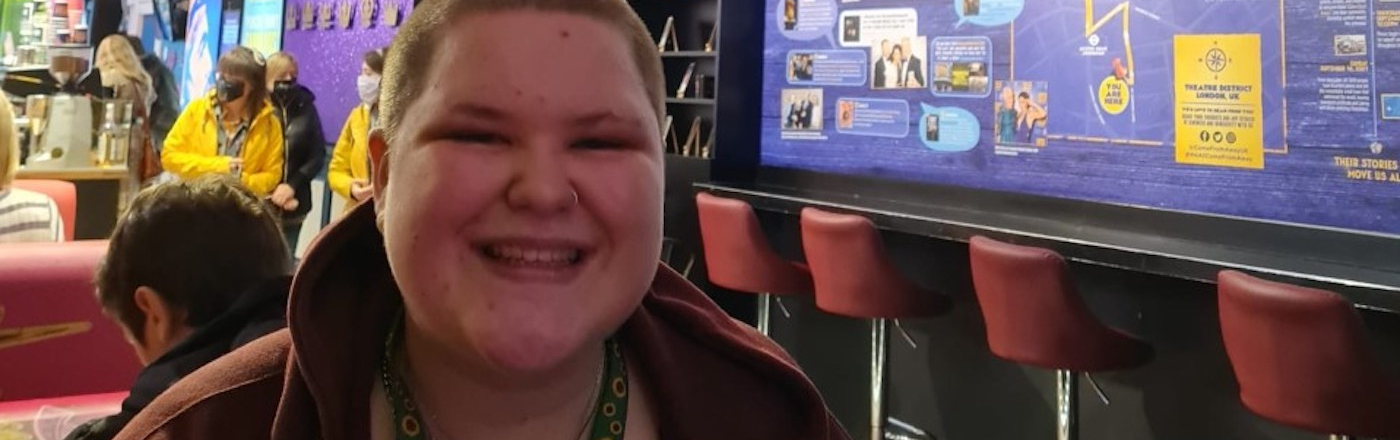
Aimee, 18, a Hidden Disabilities Sunflower wearer who has experienced symptoms of endometriosis since age 11, tells us of her painful path to diagnosis and treatment:
“When I first went to my GP about it, I was just put on the pill because they said, “just have your periods, this will sort it out”. Then I was tried on things like metronomic acid and tranexamic acid to try to manage the pain and the bleeding.
The bleeding was really heavy. I'd get symptoms the week before my period, the week of my period and then the week after. So, for three weeks of the month, I was just completely out of it from the pain. My GP told me that it was IBS because of the bowel symptoms I was experiencing.
I had blood tests for my thyroid levels, was told to cut loads of different foods out of my diet to check for intolerances. So, the GP really focused on the bowel issues themselves, rather than the timing of them - these bowel issues were only occurring on the week of my period. So, I ended up doing my own research and I found out about endometriosis online.
When I mentioned it to my GP he just said, “No, you're too young for that. It's not that condition, you're too young.” . . .I missed a lot of time out of school because of not only the pain, and the sickness caused by my bowel issues, but also the affect it was having on my mental health, not being listened to or believed.
It wasn't until I was 13 that I was finally referred to a paediatrician and then a gynaecologist who booked me in for a laparoscopy straightaway.
When I got diagnosed, I actually cried and I was like, wow, somebody has found a reason for this because you start to think when you're being dismissed so much, you start to think, oh, is it in my head? You start to question yourself.”


Gemma, a volunteer leader for the charity Endometriosis UK, had a similar experience to Aimee in terms of struggling to get a diagnosis. In fact, despite Gemma first experiencing symptoms at the age of 15, she wasn't diagnosed until she was 36 years old:
“So, I'm 41 now and I started the fight when I was 15. Back and forward to doctors. Eventually I was referred to a gynaecologist who tried to tell me it was all in my head as I'd lost my mum at a young age to ovarian cancer. So, clinicians were always putting it down to me being a worrier and thinking that because my mum passed away of ovarian cancer it was going to happen to me, that it was all in my head but I knew it wasn't in my head. So, I fought and fought and I was put on antidepressants. I was made to see psychologists and just kind of made to feel like I was losing the plot a bit.
And then eventually I agreed to do a drug trial. So, I was put on gabapentin, a drug used to treat epilepsy and nerve pain. During the trial you were working your way up to taking 12 gabapentin tablets a day and the trial was going really well until I had the 12th tablet and another week or two after that I just started collapsing. So I got in touch with the hospital was taken off them immediately and was referred for a laparoscopy. My first laparoscopy which confirmed I had endometriosis; I was 36.”
“When I was diagnosed, it was honestly one of the best days of my life because I was finally believed! That at last I could prove to them that I was never making all this up and that it was real. And to go through that for 20 odd years plus, it was really difficult.”
Why are so many women with endometriosis not being heard?
Despite endometriosis affecting approximately 1 in 10 women, putting the condition on a similar scale to diabetes, there is a huge lack of research and funding for a disease that affects so many women.
Historically, there has been limited investment in research into women’s health in general, but there’s been so little investment in research into endometriosis that we don’t even know what causes it, and without knowing the cause, a cure cannot be found. To improve options for diagnosis, care and support, and to enable those with the disease to best manage living with endometriosis, vital investment in research into the cause, treatment, management options, and diagnosis is needed.
There is no screening test for endometriosis. Until you are referred for a laparoscopy there is no way to confirm you have the condition. Because endometriosis can affect so many parts of the body — including the vagina and rectum, intestines, bladder, and diaphragm — doctors may misdiagnose it as a different chronic condition.
As Aimee tells us: “Where you've got such a complex overlapping of these sorts of symptoms and conditions it's really difficult to manage, diagnose and treat. I'm still trying to work out if its endo found on my bowel, are the bowel symptoms related or if they're a separate condition because things like colitis and Crohn's run in my family and then with the bladder, that started happening about a month and a half ago. So that's a relatively new thing that they don't have any reason why that's happened. It just happened out of the blue. So, with all the symptoms overlapping, it's really hard to work out what symptoms are from what issue and try and manage them.”
The misdiagnoses and wide array of symptoms may contribute to how long it takes healthcare professionals to diagnose this condition. Yet the complexity of endometriosis symptoms is only half of the story when it comes to the delays in diagnosing the condition. When women seek help for chronic pain associated with, or triggered by, their periods, they often hear that this experience is “normal,” just a “bad period” that they have to find ways to cope with.
The endo postcode lottery
Where you live will determine whether or not you will have access to an endometriosis specialist. While there are many general gynaecological specialists, there is a shortage of endometriosis consultants here in the UK, when compared to the amount of people requiring treatment for the condition.
Gemma tells us: “We've got girls in the support group that are paying to go private now and we've got one girl who's actually travelling to Turkey to get a hysterectomy because she just can't get any treatment here in the UK. Which is really quite scary, the lengths that people are having to go to, to just get some relief from this condition.”
When patients finally make it to the top of NHS waiting lists and are admitted for laparoscopy treatment to remove the endometriosis that has formed on organs within the body, it is often performed by a general gynaecologist who won't always be able to successfully remove it. Most gynaecologists do not have the specialist training to remove the tissue they see, which in severe cases is often very difficult to access. It often involves the bowel or bladder, which are not parts of the body gynaecologists usually deal with. This means that treatment often fails and the patient remains living in pain and needs to start the consultation process all over again to receive further treatment.
As Aimee tells us: “I had my laparoscopy when I was 14, they found endometriosis on my left pelvic sidewall, my left ovary and my pouch of Douglas. But because a general gynaecologist performed the procedure, not an endo specialist, they had to leave the endometriosis in the pouch of Douglas. I had some relief for about a year or two.
And then over time the symptoms started building back up again. I tried to get assigned back to the gynaecologist at my hospital, but the wait times were really long, so it was just a case of trying to manage it with my GP. About a year ago I saw a private endometriosis specialist. I had another laparoscopy and they found endo had returned on my bowels, the pouch of Douglas endo was still there, I had a four-centimetre cyst on my right ovary and the left pelvic sidewall endo had also returned.”
How can wearing the Hidden Disabilities Sunflower help?
Aimee originally got her Hidden Disabilities Sunflower lanyard to support her as she made her way through security at Gatwick airport to help explain why she was carrying medication. Since then, she's found that it helps her in everyday life too:
“I started wearing the Hidden Disabilities Sunflower in supermarkets and other shops. And it really does help if I have days where my pain is severe and I just need to crouch down for a minute and let the intense pain ride out. And it just means that shop staff who can recognise it are able to say, “Oh”, see if I need somewhere to sit down or anything. And it just makes me feel more comfortable going out and knowing that those people are going to understand that you've got something going on that they can't see.”
Support groups & Endometriosis UK
If you or someone you know is affected by endometriosis, joining a support group or accessing more information may help.
Endometriosis UK - work to improve the lives of people affected by endometriosis and to decrease the impact it has on those with the condition and their families and friends. Their Support Network provides vital, emotional support and information to those who have endometriosis through the support groups and helpline, enabling people to understand their disease and take control of their condition.